A steady rain is pouring as a white minibus idles on the edge of a health center parking lot in Deer Park, waiting for the final few patients to step on board this Thursday morning in late February.
Renovated to include a makeshift doctor's office at the back, complete with a reclined medical chair and small sink, the bus offers essential treatment closer to home for many who live north of Spokane.
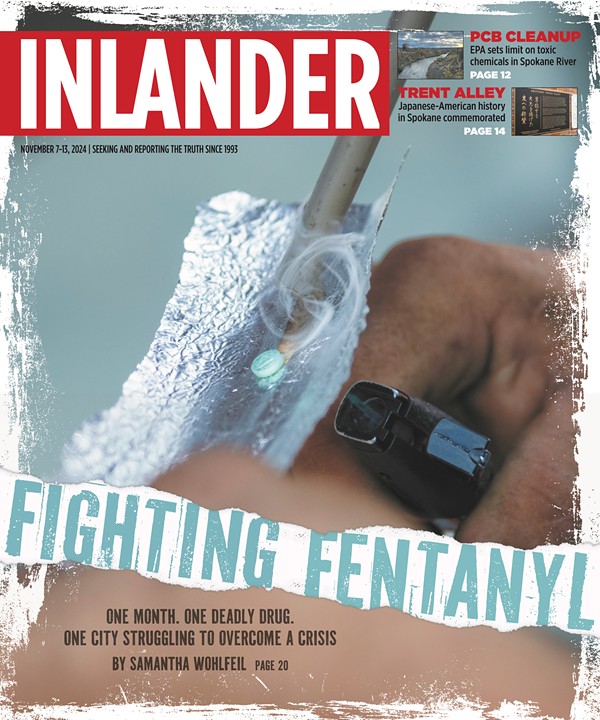
Most patients aren't there to see a doctor. Instead, they take turns boarding the bus one by one, stopping at a small window in the aisle to tell a staff member their name and patient ID number so they can receive their daily dose of methadone.
Opioid treatment programs for those with substance use disorder, or, more specifically, opioid use disorder, typically require patients to come in daily to get their medication-assisted treatment.
It can take time to earn the right to get take-home doses, and if there isn't a program nearby, it can take hours out of each day to simply drive to a treatment program, wait in line, get that day's dose, and head to work or come home.
But recently, some programs like this mobile clinic operated by Acadia Healthcare have been able to bring that treatment closer to rural residents.
Since last June, this bus has made the 40-minute trip from Spokane each morning, Monday through Friday, to set up in the parking lot of an urgent care that's just off the main drag through Deer Park.
That's a big deal for people like Robert Edwards, 53, who has been able to receive treatment here since September.
Edwards says that since his initial intake and evaluation at Acadia's brick-and-mortar opioid treatment program on East Trent Avenue in Spokane, which took about four hours, he's been able to receive care in Deer Park, making it much easier to remain in treatment. It's near his home and only takes a few minutes each day now that he's established.
"The car that I had, the transmission went out in it, so thankfully my mom is allowing me to use her car," Edwards says. "My youngest is still in school, so to get him to school and then try to get all the way down to Trent in traffic, every day, it can be done, but this just made everything so much more convenient and more possible to stay committed with the program."
After he broke his back in 1999, Edwards says, he was on prescribed pain medication for years, until doctors became more reluctant to provide them, recognizing that the meds were creating an addiction epidemic.
"I was never a drug user [before that]," Edwards says. "That led to exploring other options, and that pretty much ruined my life from there."
About five years ago, he says he started using heroin and then switched to fentanyl after heroin became difficult to find.
The treatment program has offered him stability. Medication-assisted treatment helps with pain relief and curbs cravings without getting users "high." The program also includes ongoing counseling and peer therapy to help address the shame and stress that come with addiction and recovery.
"I was extremely ashamed," Edwards says, noting it took him a long time to talk to his family about his struggles. "I shouldn't feel ashamed, because I've made huge strides to change my life around. I see light at the end of the tunnel, where before I never did."
Now, providers are excited that new federal rules set to take effect next month will make it even easier for more companies to invest in similar mobile clinics that can increase treatment access wherever there's a need.
NEW GUIDANCE
In the last two years or so, regulatory clarity enabled companies like Acadia to take off with the mobile clinic concept, says Dr. Nasser Khan, the operations group president for Acadia's Comprehensive Treatment Center division.
With seven mobile clinics in multiple states, Acadia is one of the largest operators of mobile opioid treatment programs in the country, Khan says. They plan to double the number of mobile units by the end of the year.
They operate in somewhat of a hub-and-spoke model, with mobile units dispatched from a main clinic. Each day, the bus that offers treatment in Deer Park is driven there in the morning, returning each afternoon to Acadia's clinic in Spokane, where medication is stored securely inside the building.
"[They] are located in communities that are remote, rural or otherwise underserved," Khan says. "The truth is for the majority of patients there still is a need for services that require that daily visit to the clinic. It's not just dispensing the medication, it's the other service the clinic is providing as well. ... The mobile vans fill in that important gap."
On Jan. 31, the Substance Abuse and Mental Health Services Administration released the final version of updated federal rules for opioid treatment programs, which will take effect on April 2. It's the first major update in about two decades.
The update enshrines some of the leeway that was given on an emergency basis during the pandemic.
One of the biggest rule changes will allow providers more ability to determine when someone is clinically ready to receive take-home doses, Khan says.
Aside from weekend doses, which are available from the time people start, it previously could take 90 days in treatment for patients to earn just one take-home dose of methadone, says Jason Kletter, president of BayMark Health Services, in an email. Kletter is also a spokesperson for "Program, not a pill," a campaign to expand medication-assisted treatment nationwide.
With the new rules, providers can decide if someone should be eligible for multiple weeks of take-homes from the beginning of their care.
"It's really accelerated and normalized that take-homes are an important part of the care delivery for clinically appropriate patients," Khan says.
Another change makes it clear that mobile clinics can operate as full opioid treatment centers.
Previously they were viewed more as satellite operations that mostly provided medication. Now, the rules clarify that the mobile clinics can be used for everything from the intake process (which can be done via telehealth) to counseling as well.
That doesn't mean that patients won't need to visit the main clinic from time to time, Khan says, but it allows companies to more fully utilize the vans or buses.
"This is intended to bring services on a smaller scale, but still a complete set of services, out into communities," Khan says.
For new patients in the Deer Park area, that now means they won't need to drive to Spokane to do their intake, but can start the process right on the bus.
Currently, there are about 50 people in the program there, and there's plenty of room to take on more patients, says Ashleigh Yanzick, a regional director in training for Acadia. They accept all major insurance, and for those who still need to pay out of pocket, it's about $100 per week.
Another attempt to increase access to methadone is also working its way through Congress. The Modernizing Opioid Treatment Access Act would allow doctors to prescribe patients methadone that could be picked up at pharmacies.
But Dr. Benjamin Nordstrom, the chief medical officer at Behavioral Health Group — the nation's largest network of accredited outpatient opioid treatment centers — says that while the legislation promises to increase rural access, it likely won't change anything in practice.
That's because it would specifically give that prescribing ability to board-certified addiction physicians. Nordstrom says that 87% of the population already lives within adequate distance of an opioid treatment program, so the focus is on how best to serve that other 13%. If they don't have a doctor with that specialty nearby, they'll still be out of luck.
"This is consuming a huge amount of bandwidth for something that's just not going to have a material impact. It's a blown opportunity," Nordstrom says. "The time and attention would be better spent trying to figure out ways to improve economic access to treatment."
REDUCING STIGMA
One of the biggest stigmas that remains, even among providers, is the idea that staying on methadone for an extended period of time is somehow just replacing a drug with a drug, Khan says.
Typically, "graduating" from a methadone program into abstinence isn't a clinical metric that's considered important, he says. It's a medication that's treating a chronic disease.
"It's OK to take a medication for a chronic disease, potentially if needed, for life," Khan says. "We try to use the analogy of comparing it to diabetes. ... If you require insulin for treatment of that chronic disease for your whole life, there's nothing wrong with that."
If patients are successfully no longer using illicit substances, continue to remain engaged in a program and wish to remain on methadone, that's a success, Khan says.
Jennifer, who asked to only go by her first name, says the Deer Park bus has helped her for the last four months. She previously participated in medication-assisted treatment in Spokane Valley several years ago, and got off of methadone after a year, which was her goal.
But after she realized she was starting to look for pain medication again for pain related to her job and an old workplace injury, she decided to go back into treatment and found the facility that's closer to her home in the Colbert area.
"It's just another medication that you're taking. ... You're not getting high from it," she says. "That whole addiction piece is not here. It's my medicine and that's where it's at, and thankfully I've been able to keep it that way."
Darren Thompson, 48, who started treatment in December, was previously traveling from Loon Lake to a program in Spokane when he was able to transfer to the closer location. He had a bad car accident in 1997 and was put on pain medication for years. About a year ago, he says he started using "blues" that he thought were oxycodone, but later learned were fentanyl.
"The staff and everybody is just really super nice, and it's really easy to talk to them," Thompson says.
Edwards says the harm-reduction model is key. He didn't have to worry that he'd be immediately kicked out of the program while he was transitioning from illicit drug use to the legal methadone if and when those substances showed up on a urinalysis test, which all patients are regularly subjected to. He's been through precipitated (immediate) withdrawal before, which scared him when he first decided to try the program, but he found they were understanding.
"It's serious when it needs to be, but it's also comforting to know they don't look at you differently," Edwards says. "Don't be afraid to come ask for help." ♦
Editor's Note: This story was updated on March 7, 2024 to clarify Dr. Khan's title.