While chemists have discovered an amazing amount of information about the many complex combinations of atoms that make up the world around us, there's still much to learn about how certain compounds are biosynthesized — in other words, how they're organically created in living things.
For decades, that's been the focus of Jennifer Shepherd, a professor of chemistry and biochemistry at Gonzaga University who was recently named the interim dean of the School of Engineering and Applied Science for the upcoming school year.
When she first started in the field as a master's student in the '90s, Shepherd says she helped UCLA researchers who were trying to figure out the enzymes needed to create a chemical compound called ubiquinone.
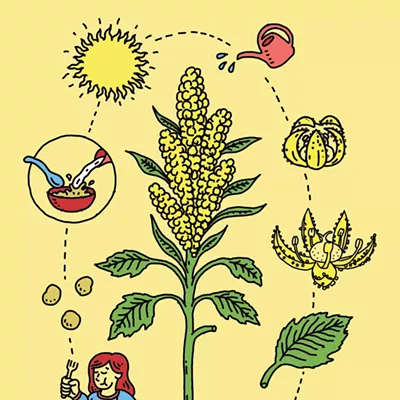
Ubiquinone is found in most living organisms and it's essential in the energy production and transfer process within our cells (in the mitochondria, for those who remember their high school science classes). Ubiquinone in humans is also called Coenzyme Q10, or CoQ10, which you can now find in the supplement aisle at the grocery store.
When she started teaching at Gonzaga more than 25 years ago, Shepherd began researching a highly similar compound called rhodoquinone, or RQ, that's made by parasites and microbes for essentially the same purpose.
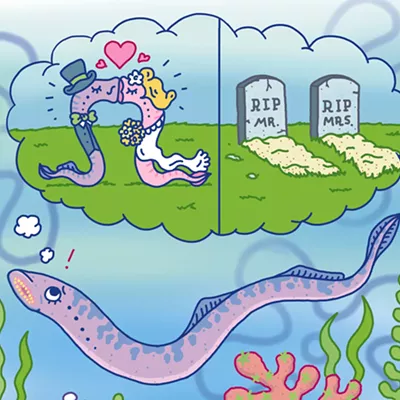
The major difference is that while ubiquinone helps create energy in oxygen-rich environments, the rhodoquinone found in parasites helps them create energy in anaerobic environments where there's a lack of oxygen, enabling them to thrive in places like our guts.
"I've spent pretty much the majority of my career trying to figure out how these organisms make rhodoquinone," Shepherd says. "The enzymes that are needed to make it, those are selective targets that we can try to inhibit or shut down."
The goal for researchers is to create new medications targeting those enzymes to fight parasitic infections.
Currently, there are only a handful of drugs on the market to treat parasitic worms, and they've remained the same for decades, so parasites are becoming more resistant to them.
Shepherd has experienced firsthand how taking those medications is fairly commonplace in developing countries such as Ghana, where she adopted three children and has traveled on many occasions. Because the infections can't be avoided there, Shepherd says that many people take antiparasitics regularly.
"You could just walk into a pharmacy and buy the treatment," Shepherd says. "Everyone has them, you can't avoid it. It's in the soil, it's in the water. You can be as careful as you want, but in the villages and at the orphanages that we were at it was kind of a monthly routine, a deworming."
Each year, more than 3.5 billion people globally are affected by intestinal parasitic infections, and more than 200,000 people die from those infections, according to 2021 research published by the National Library of Medicine, part of the National Institutes of Health.
Shepherd's team is working to find solutions.
Early on, Shepherd says her team discovered a simple way that microbes use a single enzyme to convert ubiquinone into rhodoquinone. While that initially seemed promising, it turned out that it didn't apply to parasites, which use a different method.
It took about a decade for Shepherd and other researchers to figure out one of the chemical pathways that parasites use to produce RQ.
Since then, Shepherd's Gonzaga team has worked with researchers in Uruguay and Canada to move that work forward.
Most recently, a team from the University of Toronto has been developing drug candidates that might help stop RQ production.
Gonzaga's team helps figure out how well the drugs work by analyzing batches of C. elegans worms (which aren't parasitic, but similarly create RQ) that have been treated with the drug candidates. The team processes the dried worm samples, extracting the fatty compounds where RQ can be found, and then using a mass spectrometer to see how much of the compound is present.
"They have drug candidates that they're giving to their worms, and then they're having us do the actual analysis to see if they are knocking out or reducing the ability to make rhodoquinone," Shepherd says. "We found some promising candidates."
Now, the collaborators are working to verify the drugs' effectiveness and figure out exactly how they work.
"We know it reduces the amount of rhodoquinone, but we don't know how," Shepherd says. "They're trying to figure out what enzyme in this pathway is being inhibited."
Once that becomes clear, it's possible the drugs could move to clinical testing and start the long process of getting approved for use.
In the meantime, people and livestock are stuck with the current limited options.
"That's been a problem: [for] livestock that get the infections in the U.S. and other countries, [the parasites have] definitely become resistant to the drugs," Shepherd says. "For humans, if we don't come up with other options, it's going to be the same thing." ♦